How often do patients experience worsened injuries from medical care following an accident?
James K. Sadigh reports that treatment-related complications arise infrequently but significantly, occurring in at least two dozen cases over 35 years. One notable example involved a woman who dislocated her shoulder after tripping at a restaurant due to negligence. Emergency room delays—caused by an orthopedic surgeon’s pre-planned vacation—prevented timely reduction. Stabilization over several days rendered non-surgical correction impossible, necessitating open surgery. This escalated medical costs from approximately $10,000 to six figures and transformed case value from $30,000–$50,000 to a high six-figure settlement.
Who bears responsibility when medical errors aggravate accident injuries?
Legal precedent holds the original at-fault party liable for foreseeable subsequent harm, including medical negligence. James K. Sadigh successfully applied this principle in the restaurant slip-and-fall case. The settlement covered full damages, including surgical costs. In exchange, the client assigned malpractice rights to the restaurant, enabling their pursuit of reimbursement from the hospital. This streamlined recovery while preserving client compensation.
What steps should patients take if they suspect medical malpractice after an accident?
California’s Medical Injury Compensation Reform Act (MICRA) governs such claims. James K. Sadigh advises providing written 90-day notice to healthcare providers, allowing record production and settlement exploration. Patients must avoid direct confrontation to prevent self-incriminating statements or record alterations. Securing complete medical files first enables informed legal strategy.
How can patients distinguish medical malpractice from unavoidable complications?
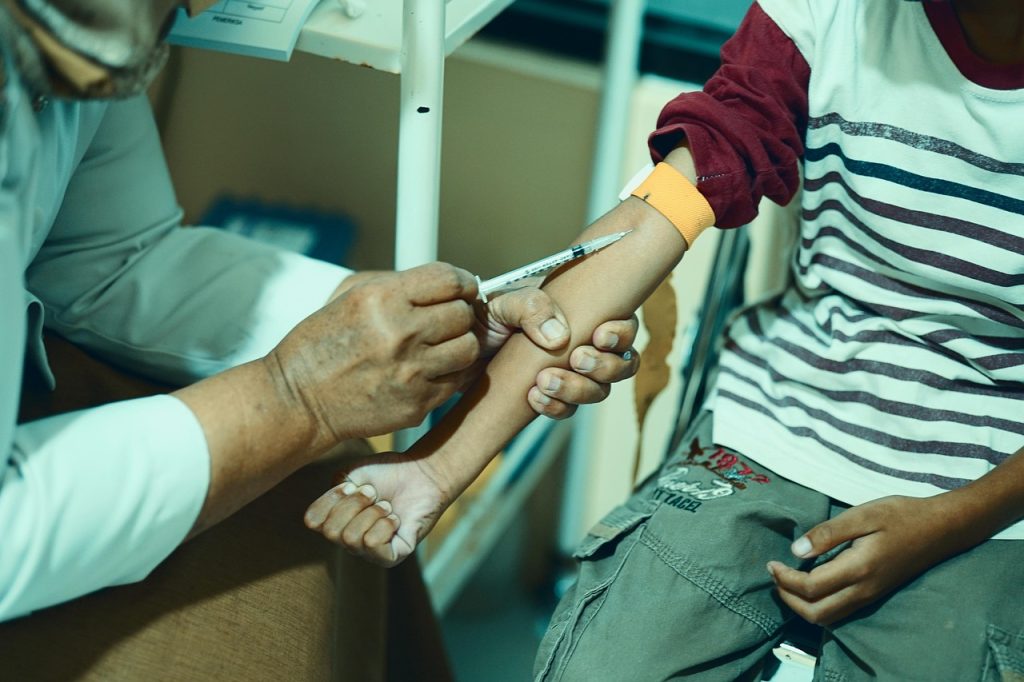
Expert consultation proves essential. James K. Sadigh retains specialists matching the treating provider’s field—chiropractors review chiropractor cases, neurologists assess neurological errors. One blood draw case initially appeared negligent due to arm numbness, but experts determined delayed intervention constituted the true malpractice; untreated nerve damage within the critical 60-day window caused permanent sensory loss. Another hysterectomy patient developed sepsis; urinary tract injury represented a known risk, but failure to hospitalize promptly upon fever onset established negligence.
Why do patients hesitate to challenge medical providers, and how can they overcome this?
Trust in healthcare professionals runs deep, and most physicians deliver excellent care. James K. Sadigh employs psychological guidance to reframe claims as preventive measures. Pursuing valid cases protects future patients from similar errors, transcending mere compensation. One family sought accountability after their mother died from a defective syringe injecting air during heart attack treatment; hospital staff ignored manufacturer recall notices. Such outcomes drive systemic improvements.
When should accident victims pursue separate medical malpractice claims?
James K. Sadigh evaluates insurance limits of the original at-fault party. Adequate coverage allows consolidation—faster, simpler recovery. Limited policies (e.g., $25,000) against inflated damages ($250,000+) necessitate separate malpractice actions. However, these cases demand early expert retention, costing $35,000–$40,000 minimum. MICRA caps attorney fees on sliding scales; smaller recoveries yield minimal client proceeds after costs.
How do personal injury and medical malpractice cases strategically overlap?
Consolidation under sufficient original liability coverage accelerates resolution. James K. Sadigh prioritizes single-case efficiency when possible. Separate malpractice litigation requires substantial evidence of deviation from care standards, proven via costly specialists. Strategic decisions hinge on policy limits, damage escalation, and net client recovery potential.